Human Rabies Vaccine: A Life-Saving Shield We Often Overlook
When we think of deadly diseases, rabies often takes a backseat in our modern-day worries. Yet, this ancient and terrifying virus still claims nearly 59,000 lives every year, primarily in areas with limited access to healthcare. What’s more heartbreaking? Almost every one of these deaths could have been completely prevented — with timely administration of the human rabies vaccine.
So, why aren’t we talking more about this lifesaving solution? And what makes the human rabies vaccine such an unsung hero in the world of public health?
Let’s explore.
Rabies: A Silent Killer That Strikes Fast
Rabies is caused by a virus transmitted through the saliva of infected animals — most commonly through dog bites. Once symptoms start, rabies is almost always fatal. There is no effective cure once it reaches the nervous system.
But here’s the game-changer: The disease is entirely preventable — thanks to a simple series of vaccines that can be given either before or after potential exposure.
Understanding the Human Rabies Vaccine
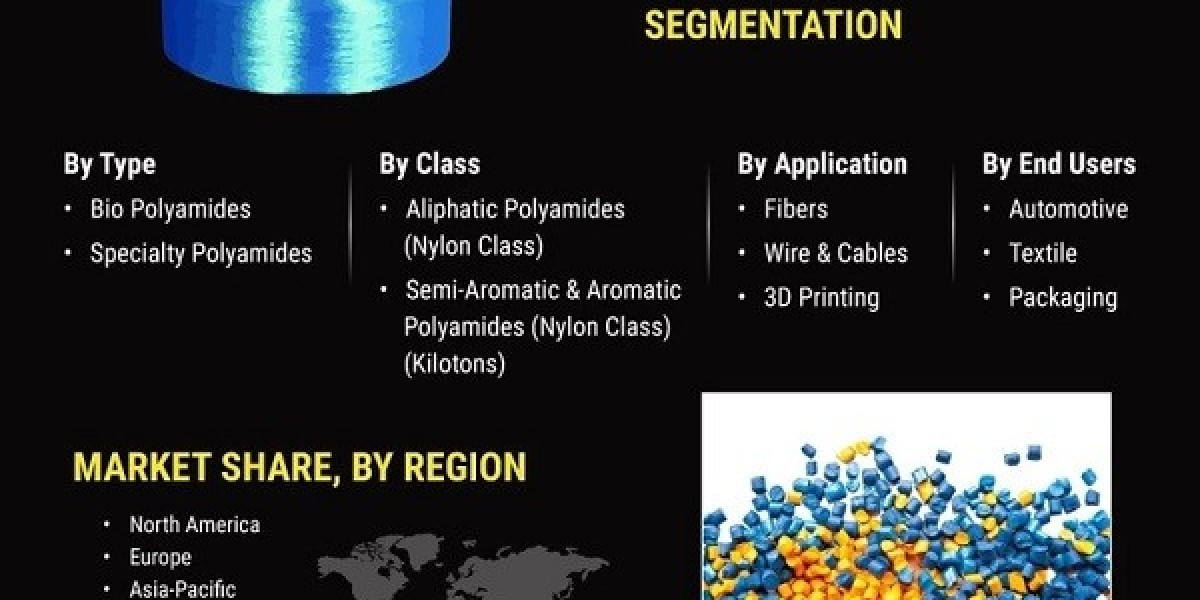
The human rabies vaccine comes in two key forms:
Pre-exposure prophylaxis (PrEP): Given to people at high risk of exposure — such as veterinarians, lab workers, animal handlers, or travelers to rabies-endemic regions.
Post-exposure prophylaxis (PEP): Administered after a suspected exposure — like a bite from a stray or unvaccinated animal.
It’s not a one-size-fits-all solution. Depending on the situation, a healthcare provider might recommend a combination of rabies immunoglobulin (for immediate protection) along with the vaccine series for long-term immunity.
Why the Human Touch Matters
Let’s take a step back and think about the human side of this story.
Imagine a child playing outside, laughing as a stray dog chases after the ball she kicked. That moment turns into a nightmare with one swift bite. Her parents panic, not knowing whether the animal had rabies or what steps to take next.
In such moments of fear and confusion, access to accurate information and prompt medical care — especially a rabies vaccine — makes all the difference between life and death.
Unfortunately, in many low-resource areas, vaccines are scarce, and even basic awareness is limited. This is where education, policy support, and public health infrastructure need to catch up with medical science.
A Global Health Challenge with Local Impact
You might think rabies is a problem far removed from urban life or developed countries. But rabies doesn’t discriminate. In rural communities, particularly in parts of Asia and Africa, the burden remains enormous due to:
Limited access to timely vaccination after exposure.
Widespread populations of stray animals.
Lack of public awareness about post-bite protocols.
According to the World Health Organization (WHO), children under 15 account for 40% of all rabies deaths — a gut-wrenching statistic that underscores the urgency of scaling vaccine accessibility.
Innovation and Hope: What’s Changing in 2025
Thankfully, we are seeing progress.
In 2025, the landscape of rabies prevention is shifting. Newer versions of the human rabies vaccine are being developed that:
Require fewer doses, reducing the burden on patients and health systems.
Offer improved thermal stability, meaning they don’t always need refrigeration — ideal for remote areas.
Are part of global health initiatives, such as the "Zero by 30" campaign by WHO, aiming for zero human deaths from dog-mediated rabies by 2030.
Additionally, community-based outreach programs and mobile vaccination clinics are playing a transformative role in underserved regions.
When Prevention Becomes a Responsibility
Rabies prevention isn’t just a medical topic — it’s a social responsibility.
Here’s how we can all contribute:
Pet owners must ensure their animals are vaccinated.
Travelers to high-risk areas should consult doctors for pre-exposure shots.
Parents and schools should teach children how to avoid risky encounters with stray animals.
Local governments need to invest in public health infrastructure and awareness campaigns.
Ultimately, the human rabies vaccine isn’t just a sterile product stored in a medical fridge — it’s a symbol of hope, prevention, and compassion. It represents the power of science to save lives when combined with proactive policies and community support.
Browse More Reports: